Why Experts Are Exploring Ketogenic Therapy For Mental Health
Authored by Jennifer Sweenie via The Epoch Times (emphasis ours),
Research suggests that metabolic health may play an essential role in mental well-being.
After years of therapies, medications, retreats, and self-exploration, Michael, a former nutrition client of mine, had resigned himself to a familiar low-grade depression and anxiety he’d carried since childhood. He accepted it as part of who he was. However, following Michael’s debilitating autoimmune diagnosis, a friend mentioned that changing her own diet had put her condition into remission. In physical pain on top of his depression, Michael decided to try an elimination diet.
Michael made several key changes to his eating—he cut out processed foods, refined carbs, and sugar, while adding healthy fats, increasing protein, and focusing on whole foods, including vegetables and fruit.
His physical health improved within a few months—and most strikingly, his depression lifted in just one month.
“I felt like life had come back into me. My mind was clear and my apathy gone. I never thought I would feel this happy again.”
* * *
ATTENTION: Buy some meat before free shipping goes away Sunday night... Several items already sold out.
Just the Steaks (10 lbs) // Filet Mignon and other goodies (11 lbs) // Ground Beef (10 lbs, on sale in addition to free shipping) // Texas Lasagna & Meatballs (clean comfort food... holy crap it's good) // Beef, Chick & Pork Trio
* * *
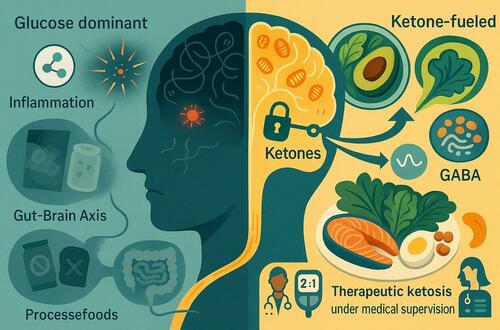
For decades, psychiatry has focused on chemical imbalances in the brain. Now, growing research suggests that overall metabolic health—how efficiently the body produces and uses energy—may play an equally important role in mental well-being. That’s why scientists are now exploring therapeutic ketosis, a medically supervised ketogenic diet, as a potential tool for conditions ranging from depression to bipolar disorder.
This promising approach also sheds light on how everyday food choices can influence both metabolic health and mental well-being, raising a timely question: How can we eat to best support our minds and moods?
The Science of Metabolic PsychiatryMetabolic psychiatry is an emerging field that examines how diet and inflammation affect brain energy metabolism, which in turn affects mood. The brain primarily runs on glucose, but it can also use ketones as an alternative fuel when glucose is low.
“Most of the important mechanisms are not about neurotransmitters at all. It’s about ketones bypassing brain insulin resistance and improving mitochondrial health,” Dr. Matthew Bernstein, a board-certified psychiatrist and leading voice in metabolic psychiatry, told The Epoch Times.
About one-third of people with serious mental illnesses meet the criteria for metabolic syndrome, according to the results of one cross-sectional study, highlighting the overlap between physical and mental conditions.
The overlap has prompted research into the underlying mechanisms. Emerging evidence suggests that when cells lack sufficient energy or oxygen, their mitochondria can malfunction, leading to brain inflammation and potentially affecting mental function.
A preclinical study published in Cell in April found that inflammatory molecules can influence anxiety by acting on specific brain cells. A 2025 review published in Healthcare the same month suggests neuroinflammation may link psychiatric and systemic disease, though more studies are needed to clarify causality.
Metabolic Psychiatry in PracticeThe research suggests that metabolism is the common thread linking psychiatric illness, brain energy regulation, and inflammation. Early findings are promising and point to a future where psychiatry addresses the full metabolic context of the brain.
“This is moving really fast. Metabolic psychiatry has a good group of people behind it from many disciplines, and therefore, we are pushing ahead with the randomized controlled trials,” Erin Louise Bellamy, a metabolic psychiatry clinician and researcher, and expert in ketogenic therapy for depression, told The Epoch Times.
A clinical trial published in The Journal of Clinical Psychiatry found that improving insulin sensitivity alone reduced depressive symptoms in patients with treatment-resistant bipolar depression. The researchers used metformin to improve insulin resistance, suggesting that targeting metabolic dysfunction may help improve mood.
Given metabolism’s role in brain function, ketogenic therapy is being explored as a potential tool. A pilot study published in Translational Psychiatry in September found that in college students with major depressive disorder and already receiving treatment, following a well‑formulated ketogenic diet for 10 to 12 weeks was associated with approximately 70 percent reductions in depression symptoms and improvements in cognition and well‑being.
A review published in Current Treatment Options in Psychiatry, involving nearly 2,000 people, concluded that ketogenic diets appear safe, feasible, and effective in targeting inflammation, mitochondrial dysfunction, and metabolic dysregulation.
Understanding the metabolic influences on the brain sets the stage for exploring dietary interventions that support mental health.
Therapeutic KetosisTherapeutic ketosis is a medically supervised ketogenic intervention that shifts the brain from relying on glucose to using ketones, produced when fat is broken down in the absence of carbohydrates. First developed nearly a century ago to treat drug-resistant epilepsy, it is now being explored for mood and psychiatric disorders.
The overarching theory of therapeutic ketosis is that it improves metabolism by reducing inflammation, stabilizing blood sugar, and countering insulin resistance, while improving mitochondrial health—the “batteries” that make us tick and work.
“We are fixing that [mitochondria], or at least giving it some time out away from all the blood sugar spikes, to get healthy again,” Bellamy said.
Unlike popular keto diets marketed for weight loss and convenience foods, therapeutic ketosis uses precise macronutrient ratios, monitors ketone levels, and requires medical supervision. A neurologist works with a registered dietitian to prescribe a diet to a patient.
“It will be carefully calculated to change their metabolic physiology,” Dominic D’Agostino, associate professor of molecular pharmacology and physiology at the University of South Florida Morsani College of Medicine, told The Epoch Times.
Bellamy noted that fat-to-carb-plus-protein ratios can be adjusted individually, often being roughly two parts fat to one part carbs, plus protein.
A day’s diet following such a ratio might include eggs with bacon cooked in cream and butter for breakfast, a leafy green salad with chicken, avocado, and plenty of olive oil for lunch, salmon with roasted asparagus, drizzled with butter and olive oil for dinner, and a small handful of macadamia nuts or a piece of full-fat cheese if needed to maintain the ratio.
The popular keto diet carries a lot of baggage—meaning it’s often overhyped and sensationalized. People tend to focus on extreme versions, packaged treats, celebrity anecdotes, or short-term results, which can give the wrong impression of how therapeutic keto actually works, D'Agostino said.
Though research is still early, evidence suggests therapeutic ketogenic interventions may improve symptoms in depression, bipolar disorder, and anxiety. Bellamy added that ketosis targets six or seven different pathways, with each person having one or two working at any one time. As a result, ketosis can benefit many people, but the mechanisms and response can vary.
“If you elevate circulating ketones, they rapidly cross the blood-brain barrier and restore normal cerebral metabolic activity,” noted D’Agostino.
A ketogenic diet often works like a form of calorie restriction because it’s less palatable and naturally helps you feel full, so you don’t overeat like on a standard American diet, he said.
Ketones directly calm inflammatory pathways linked to psychiatric disorders. In the brain, they provide an alternative energy source when glucose is low and boost GABA, a calming neurotransmitter, acting somewhat like a mild anti-anxiety medication.
Gut inflammation may also play a role in the mechanisms of therapeutic keto.
“There’s just not enough hard science about exactly which microbes we want and which we don’t, and which are helpful and which are not. We’re still at the infancy of learning all of that, but definitely reducing gut inflammation.” Bernstein added.
As to the long-term benefits of therapeutic ketosis, “Some people retain benefits after coming off the diet. We think it has the potential to create a healing process in the brain. If someone’s been on a ketogenic diet for a few years and they come out of ketosis, I don’t expect all their symptoms to come back immediately, he said.
You Don’t Have to Enter KetosisFor severe mental illnesses such as bipolar disorder, schizophrenia, major depression, or obsessive-compulsive disorder, medical supervision and ketosis may be needed to see significant benefits. In contrast, moderate depression, anxiety, or attentional issues may respond to less strict low-carb strategies, Bernstein said.
Diets high in refined carbs and added sugars are linked to higher rates of depression and anxiety, while diets rich in whole foods may help reduce depressive symptoms. Removing ultra-processed foods gives the body a more even playing field to improve metabolic health, Bellamy said.
She recommends returning to foods our grandparents would recognize to help stabilize blood sugar, including prioritizing animal protein, cooking with butter or coconut oil, a variety of vegetables, especially leafy greens, and choosing fattier cuts of meat.
A common question Bernstein grapples with in clinical practice is whether people can see mental health benefits from lowering inflammation through diet—cutting processed foods or eating low-carb—without committing to full therapeutic ketosis. He suggested easing in by reducing ultra-processed foods, added sugar, refined flour, and industrial refined oils, while emphasizing whole foods and vegetables. Then, consider a lower-carb or low-glycemic diet next. Habits such as regular exercise, quality sleep, circadian rhythm alignment, and mind-body practices can further support many of the same metabolic processes targeted by a ketogenic diet.
Bernstein suggested a mindset shift around eating fat: “Initially it’s about not fearing fat … That’s a whole psychological shift people need to make. There really is no good evidence that saturated fat is bad for us.”
Small interventions, such as time-restricted eating or adding MCT oil in the morning, can also help, he said.
Even a simple low-carb diet—around 100 grams of fibrous carbs from vegetables and fruits while avoiding processed grains—can deliver many of keto’s benefits, D’Agostino said.
Michael’s elimination diet was one example—he cut carbs drastically but didn’t enter ketosis, removed inflammatory foods, and increased healthy fats like coconut oil, duck fat, and tallow.
“You, as an individual, have the ability to choose how you eat and the nutrition you have day to day… all of that is within your grasp right now, and you don’t have to wait,” Bellamy said.
Always check in with your physician before making major dietary changes—including trying a ketogenic diet—especially if you take medication to manage a mental health condition.
Loading recommendations...